I have been a hospice Registered Nurse for about ten years. Hospice is similar to home health except specializing in care of the terminally ill, dying patient. A hospice nurse provides palliative care for the patient during their last months, weeks, days, or hours so they may pass in the comfort of their home and with their loved ones present. I provide comfort and dignity for the the patient and comfort for the caregiver. Following the peaceful passing of the patient I provide postmortem.
Well both honestly. yIts very easy to get cauht up and become very involved with your patient and their families. It does have a very profound effect on the psyche. It is truly a calling. That is why I am so proud to have been involved in such a profession. I know I am a nurse but all nurses have a calling. You have bad nurses and great nurses. The difference is the ones that truly seek their calling and do THAT as their career are the BETTER nurses per say. Not just anyone can do hospice. The fact that it is a calling, in my opinion, is what makes us resilient and able to rebound and turn sadness into such a profound feeling of gratification for helping your patient and being the support and educator for their loved ones that you do have a sense of fulfillment. It is hard to explain but YES it gets depressing. I had to break from it temporarily after four years of strictly seven on and seven off on call duty. It became hard for me because naturally as a nurse your job is to nurture and heal, thats why most get into the profession anyway. As a hospice provider your not healing and sending a well patient home. You know from the day of admission that you will lose your patient. Our job is to make them comfortable until inevitable death occurs. And as only a oncall RN you are the rescue in the middle of the night, weekend, and holidays, which was so very rewarding but at the same time not many "good calls" or "good visits" occur during those hours. So I missed the daily, weekly visits and bonding with the patients and the families and was only getting to deal with the death part of the process. Very sad at times.
Google hospice patients alliance
This is very interesting. That is hard to answer because I am not familiar with this invention or how it is used. A hospice patient, at a certain point would not be able to use the device, depending on how it is used. The reasons being weakness, disorientation, and eventually a comatose state. However, it probably would be a wonderful thing to present from a caregiver standpoint. Normally hospice patients in the end state are not going to catch "bugs" etc and normally at this point it is of no concern. I know that sounds horrible but what I mean is, at the point of inevitable pending death and as it nears, the focus is NOT whether or not they catch a cold or anything else, it is to have loved ones around and proper palliative care to ensure a peaceful passing. Make sense? BUT if you wanted to present that to hospice companies, try the approach for the hospice patient that is alert and oriented with lung issues, pneumonia etc to prevent spread to a caregiver and present it to suggest to caregivers. Also I would suggest to promote it for the employees, especially your CNAs that spend MORE time with the patients and families due to the job they do. It is more up close for more time due to bathing the patient etc. We all know we cannot call in everytime we have a simple cough or cold and this could easily be a good thing to be utilized by hospice providers to prevent spread of "bugs" to a patient. Use the phrase, to prevent facilitating the dying process secondary to spread of germs and infecting your patients. :)) hope this is helpful to you. Also I am a Multiple Sclerosis sufferer, our treatments break down our immune system and almost every single thing we come into contact with makes us sick. Present this invention to doctors that treat patients with autoimmune disease and cancer. Reasons, chemo and medications for autoimmune disease break down the immune system. Best of luck with this :)
I had to come back and edit this answer because if you could later come up with an idea to push for chronic lungers etc that cough even while comatose, a gadget that can be utilized for them, almost like an oxygen mask with a filter or whatever you use in the cup in a bag? Like an ambu bag? Just FYI I am no inventor haha Just hospice nurse ;)
Oh my, it happens so frequently. As protocol we get the Social Worker involved and meet with the family. We can choose to report to authorities but normally, unless it is a major issue and habitual, we opt not to have others involved. The reason is because the last thing a dying person needs is chaos and drama. They do not need to have loved ones being shipped off to jail during the dying process. One company I worked for we would remove all narcotics etc from the home and an on call nurse HAD to make visit each time the patient needed medications. I have had to resort to a pain pump in the past to prevent such. Also the transdermal patches help because it is quiet difficult to turn a patient and remove a patch for self gratification. I placed the patch on my patient normally on the backside somewhere and initialed and dated it. Also I always always make the families aware that I monitor my patients' medications each visit and count them. The patches normally are five to a box and I monitored those as well. Sorry for the delay I have been dealing with my MS and treatments.
Server / Bartender
 What's the best tip you ever got?
What's the best tip you ever got?
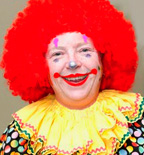
Birthday Party Clown
 OK seriously, how DOES the clown car thing work?
OK seriously, how DOES the clown car thing work?
Couples Therapist
 Does a therapist aim to "fix" the client, or just treat the client indefinitely?
Does a therapist aim to "fix" the client, or just treat the client indefinitely?
When I worked we had in services constantly to ensure compliance with state! All hospices or any medical field must provide info on how to report non compliance! I am not sure of how to ensure you get to the correct people without possibly checking that particular companys website. But there is a link
-OR-
 Login with Facebook
Login with Facebook (max 20 characters - letters, numbers, and underscores only. Note that your username is private, and you have the option to choose an alias when asking questions or hosting a Q&A.)
(A valid e-mail address is required. Your e-mail will not be shared with anyone.)
(min 5 characters)
By checking this box, you acknowledge that you have read and agree to Jobstr.com’s Terms and Privacy Policy.
-OR-
 Register with Facebook
Register with Facebook(Don't worry: you'll be able to choose an alias when asking questions or hosting a Q&A.)